Restraint devices in nursing homes
Promote patient comfort and safety
thanks to the correct use of restraint devices
Introduction
The relevance of restraints
The topic of physical restraint of assisted people today opens a wide debate among nursing professionals, especially in the geriatric field, psychiatric and, therefore, within structures such as protected houses, nursing homes, rest homes, psychiatric wards, etc…
1.1
Protocols and procedures
Patient comfort and safety are both to be pursued during the period of restraint.
Identification of the persons who needs restraint for the treatment attendance:
- data collection for each assisted person during entrance;
- evaluation of the state of conscience of the person who must undergo therapy;
- evaluation of the cooperation level of the patient through interview;
- team evaluation on the real need of use the means of restraint




1.2
Target audience
Resources
- nurse;
- nursing evaluation form;
- nursing log.
Addressee
Patients suffering from:
- diseases borne by the S.N.C. (Alzheimer disease, dementia, Parkinson’s disease, etc.);
- liver cirrhosis;
- confusional state (in the elderly patient)
- toxic-deficiency syndromes (alcohol or narcotics);
- psychiatric diseases.
Information to the patient and his family
- explain the importance and necessity of the therapy;
- encourage the patient (make him feel you close), informing him that the restraint will be removed at the end of the therapy
Validation of the use of the means of restraint in clinical documentation of the assisted person
- medical prescription in the clinical log;
- annotation in the nursing log;
- filling in the nursing form.

1.3
Choice and use of the appropriate means of restraint
Positioning of the restraint device (e.g. bracelet):
- wrap the cuff around the patient’s wrist so that it is not too tight, securing it to the bed so that the patient has a limited range of movement.
Control
- every thirty minutes the correct positioning of the restraint device.
At the end of the treatment
- removal of the means of restraint.
Same procedure for all other means of restraint.
In hospitalized people, with health problems attributable to alteration of the state of consciousness and / or alterations in motor function, there is an high risk of accidental falls during hospitalization. This protocol is intended to prevent this occurrence.
People with behavioral disorders (psychomotor agitation, confusional state, etc.) and exuberant motor activity
- evaluate motor capacity;
- prepare a comfortable environment with soft lighting, eliminating any background noises or potentially dangerous objects;
- detection and prevention of risky situations, due to disturbance such as environmental or interpersonal intolerance;
- keep the person away from the triggering event;
- implement relational strategies with the patient;
- equip the patient with padded clothing;
- propose walks or activities to distract the patient from aggressive outburst;
- request the cooperation of relevant, familiar people (family members or known people).
Should the aforementioned strategies have not had any effect:
- evaluate the need of using means of restraint;
- choose the most appropriate means of restraint considering the situation and the patient;
- apply the means of restraint;
- the prescription must indicate: motivation, type of restraint, duration;
- inform the patient and his family about the need of restraint;
- validate the use of the means of containment in the patient clinic documentation (medical prescription);
- monitor and record any remark on the given form every 30 minutes.
People with behavioral disorders (psychomotor agitation, confusion, etc.) and limited motor activity
- evaluate motor capacity;
- prepare a comfortable environment with soft lighting, elimination of background noises and potentially dangerous objects;
- detection and prevention of risky situations, due to disturbance such as environmental or interpersonal intolerance;
- keep the person away from the triggering event;
- implement relational strategies with the patient;
- equip the patient with padded clothing;
- use orthotic supports to maintain correct posture (wheelchair belt);
- request the cooperation of relevant, familiar people (family members or known people).
Should the aforementioned strategies have not had any effect:
- evaluate the need of using means of restraint;
- choose the most appropriate means of restraint considering the situation and the patient;
- apply the means of restraint;
- validate the use of the means of containment in the patient clinic documentation (medical prescription) indicating: reasons, type of restraint, duration of treatment;
- inform the patient and his family about the need of restraint;
- monitor and record any remark on the given form every 30 minutes.

People with motor impairments: walking disorders, asthenia, etc
- Propose walking aids
- Apply orthotic supports for the correct maintenance of posture;
- Monitor the person and record remarks in the nursing log.
1.4
Use of restraint systems
Advice – Recommendations
- Choose between the Heavy Duty or Basic lines based on your needs: the Basic line is ideal for normal conditions, while the Heavy Duty line is indicated for situations in which a greater containment capacity is required (for example particularly exuberant and/or uncooperative patients).
- Restraint cannot be imposed for more than 12 consecutive hours unless extremely required due to the subject conditions.
- During the period of restraint guarantee to the patient the possibility to move and exercise for no less than 10 minutes every 2 hours (night not included).
- Evaluate every 3-4 hours the occurrence of any damaging effects directly caused by restraint, such as abrasions, bedsores, edema of the lower limbs, hematomas, etc.
Complications related to the use of restraint means
Potential damage related to incorrect use and / or prolonged means of restraint are divided into three categories:
- Mechanical trauma: strangulation, asphyxiation by compression of the rib cage, superficial soft tissue injury
- Functional and organic diseases: psychophysical deconditioning, incontinence, pressure ulcers, infections, decrease in mass, tone and muscle strength, increased osteoporosis.
- Psychosocial syndromes: stress, humiliation, depression, fear, and despair.

Patient in bed
2.0
Products
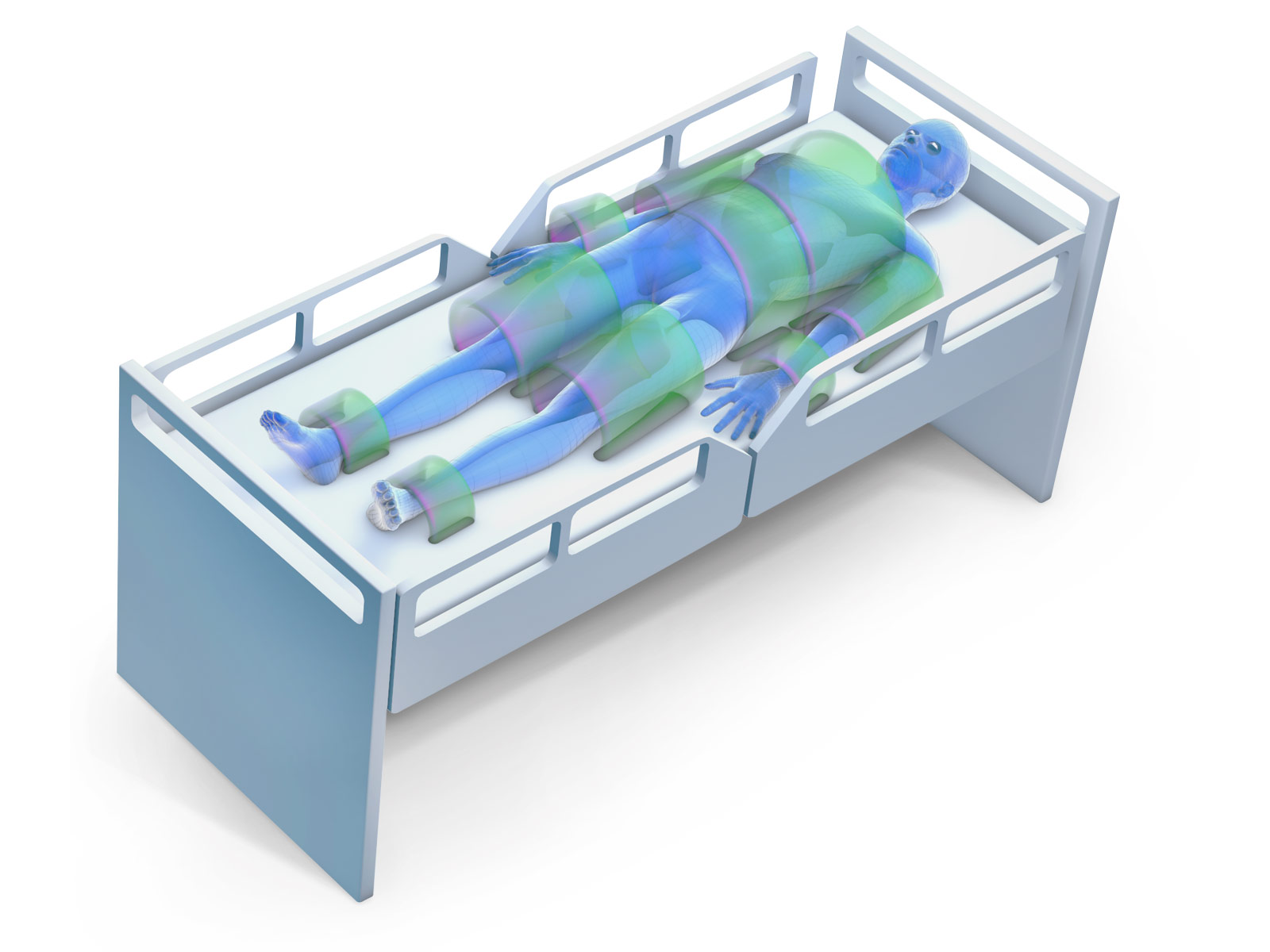
Abdominal restraint
Wrists restraint
Thighs restraint
Ankles restraint
Operational videos
Patient on wheelchair
3.0
Products

Thighs restraint
Ankles restraint